What Does Labour Look Like? The Stages of Birth Explained
You might find yourself beginning to think more about your baby’s birth as 40 weeks approaches and wondering what labour might be like. Of course, everyone’s birth journey will be unique to them, but it’s good to familiarise yourself with the stages of labour so you can better understand what might happen.
Early Labour – What You Might Notice First
When you first notice signs of early labour, you might be asking yourself ‘Is this really it?’ It’s often difficult to know whether labour has started as the early signs can be missed.
If you are less than 37 weeks pregnant, call your midwife straight away if you think you are in labour.
It is likely they will suggest that you head into hospital so you can find out if labour has begun and your next steps;
this will greatly depend on your current gestation.

During early labour (also known as the ‘latent’ phase), there is a lot happening in your body; your cervix is beginning to soften, thin and open which can lead to mild period-like cramps. Some women experience mild backache, and these sensations may come and go in an irregular pattern. You might also experience pressure in the pelvis, and you might see your mucus plug. ‘What?’ I hear you say? Yes, it doesn’t sound very pleasant because, well, it’s not! Your mucus plug is a thick, gel-like mass of mucus that seals the cervix during pregnancy to protect your growing baby from infection (amazing, right?!). As your cervix begins to open, the mucus plug might come away. You might not even notice it. But if you do spot it, it should appear clear/off-white in colour or could be slightly bloody (and as a result is sometimes referred to as a ‘bloody show’). It doesn’t always mean labour is imminent, but it does mean that your body is getting ready to birth your baby.
Will labour begin with my waters breaking?
Due to the way that labour is dramatically portrayed on the television and in films, many believe that waters breaking will be the first sign of labour and that waters will release with explosive force when you are in the middle of a supermarket or at an important event. Only 8-10% of women experience waters breaking as their first sign of labour. I was actually one of these! But I was asleep in bed and awoke to wet sheets. My waters then began to trickle for the next 12 hours so not explosive like in films!
If your waters do break early, put in a sanitary pad and monitor the colour. Your waters should be clear, or pinkish/straw-coloured. If your waters appear yellow or green in colour, or look bloody, please contact your midwife as this could indicate infection or a distressed baby. Your waters can break as a gush or as a trickle and they are likely to trickle for quite a while so be aware of this. Certain movements from you or baby can also mean that larger amounts of water can release at different points so you might find you need to change your sanitary towel often.
What should I do in early labour?
You might experience different emotions when the early signs of labour begin. There might be excitement, panic, or you might just go into a focused little bubble. However you feel, if labour is beginning, the sensations you feel might come and go for several hours or even days. There is no need to rush! If you can continue to do whatever you were doing, carry on. The best thing you can do is distract yourself so your body can continue to do what it needs to do without your mind interfering. If you were about to go to bed, go to bed! Conserving energy in the early phase of labour is essential as you’ll need it later on.
If your labour begins during the day, try to keep in an upright position and gently active as this will help baby to get into a good position for birth. In early labour, stay hydrated and fuel your body (eat slow-release energy foods little and often and also quick-release energy foods) – just like you would do if you were preparing for a sports event.
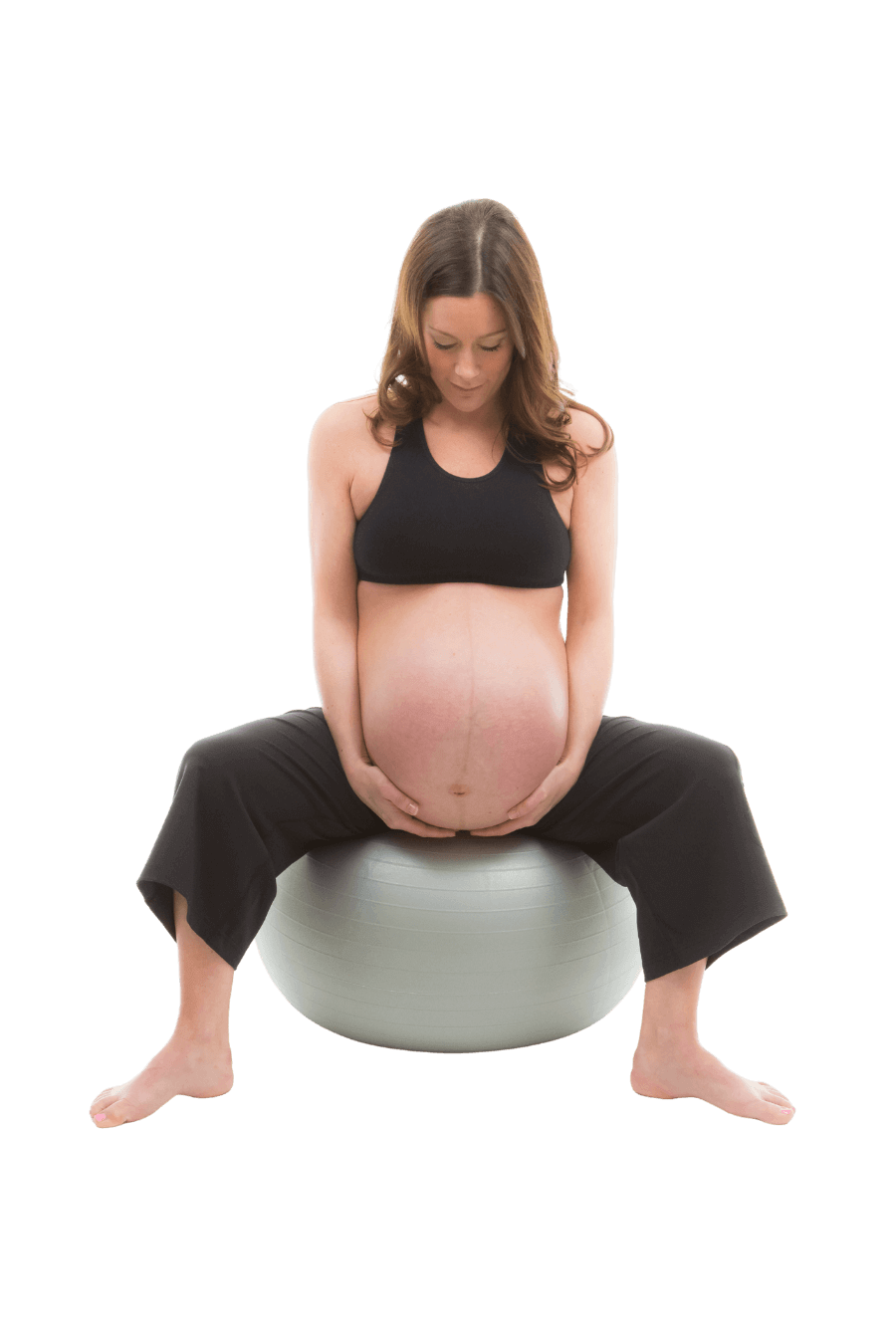
Oxytocin is the hormone that helps your labour unfold and move forward, so doing anything that encourages its release is a good idea—unless, of course, you’re really tired and were planning to go to bed, then go to bed! Rest might be exactly what your body needs. You might find comfort in a warm bath, soft music, or a relaxation script. Cuddling with your birth partner or watching something that makes you laugh can also help your body relax and open. If rest feels right, sitting on a birth ball or lying on your left side can be gentle, supportive positions. If you have a TENS machine, it may be helpful in the early stages of labour. And if you try it and don’t love the sensation at first, don’t write it off—many people find it works better later on. (For me, I hated the sensations from the TENS machine while in labour with my son and disregarded – something I wish I hadn’t done. In contrast, I found it helped immensely when I was in labour with my daughter.)
Most of all, try not to panic. You’ve got this! Focus on long, slow breaths to keep oxygen flowing and help your body stay calm. You’re also more likely to feel comfortable and safe in the privacy of your own home, where oxytocin flows most easily. Unless you need medical support, staying at home for as long as you can may help your labour progress naturally.
When Should You Call a Midwife in Cornwall or Devon?
With so much of Cornwall and Devon being rural, you might be wondering when the best time to call the midwife is, once labour has begun. It is generally advised that you call midwives when your contractions are coming around every 5 minutes and lasting around 60 seconds. If you are planning to travel to a hospital or birth centre to give birth, they might advise you to begin your journey (depending on how far you have to travel). If you are planning a home birth, the midwife will ask you how your labour is progressing and will let you know when they will be with you.
Should your waters break early in your labour, it is a good idea to call your midwife/birth centre/hospital to inform them. They might suggest you head in early for monitoring, particularly if you have tested positive for Group B Strep. Listen to advice and decide whether heading into hospital is right for you and your baby. Labour often progresses more quickly at home, so you might opt to go into hospital to be checked and then head back home after speaking to your birth team.
If your waters breaking is your first sign that baby is coming, it is most likely that you will go into labour with in 24 hours, and highly likely that labour will begin within 48 hours *. If labour does not start within this time, you will be offered induction. This is because, once the amniotic fluid has been released, there is a small increased risk of infection for your baby.
Understanding Active Labour
Active, or established labour is usually recorded as the point at which you are experiencing contractions every 3-4 minutes and these are lasting around 40-60 seconds. If you notice your contractions are beginning to form a more regular pattern, ask your birth partner to time them or use an app to record the timings so you can pass this on to your midwife. If you accept a vaginal examination (note you have to consent to these), midwives will usually record active labour as the point at which your cervix has dilated to 4cm.
If you are planning to give birth at home, midwives are likely to make their way to you once your birth partner has informed them you are experiencing regular contractions which suggest you are in active labour.
If you are planning to give birth in a birth centre or a hospital, you might find that your contractions lose a little power during your journey from home. Bright lights, conversations and having unfamiliar people around you can all also cause labour to slow. Consider taking things in your birth bag which will help you to feel calm and relaxed during labour. Setting up your birthing environment once you are in your own room is a good job for your birth partner while you focus on getting back into the zone.
What is the First Stage of Labour?
The first stage of labour is usually split into 2 parts: the latent phase and the active phase. This stage is also referred to as the ‘UP’ stage of labour. During a contraction in the ‘UP’ stage of labour, the outer layer (vertical muscles) draws up. The inner layer (horizontal muscles) relaxes. As the vertical muscles draw upward, the horizontal muscles are slowly gathered at the top of the uterus. The muscles moving in this way, along with the baby’s weight bearing down, encourages the cervix to dilate.
When you are in the first stage, midwives will monitor both you and baby by doing regular checks (with your permission). If this is your first baby, the active stage can last, on average, somewhere between 8 and 18 hours. This might seem like a long time, but remember, the sensations of labour intensify as labour progresses and rarely come on strong to begin with. If you have given birth before, it is likely that this stage will be shorter, somewhere between 5 and 12 hours.

What is Transition?
Once the muscles have drawn up, it’s time for them to work baby down and out! The muscles now switch roles. This swapping point in your labour is known as ‘transition’. Internally, there are huge hormonal changes, and you will receive a burst of adrenaline and noradrenaline. Transition will be different for everyone. You might experience a sudden increase in intensity, a feeling of pressure, and a need to bear down. This is likely to follow a pause, a decrease in the strength of your contractions, offering you a natural break to regain some energy before the next stage begins (isn’t it amazing that our bodies provide us with a natural rest?!). As a result of this, it is also often known as the ‘Rest and be Thankful Stage’. Keep calm, take some slow, deep breaths and accept hugs and words of encouragement from your birth partner. Keep that oxytocin flowing! Birth partners (and you) need to be aware that it is highly likely that you will have a slight ‘wobble’ at this point in your labour. You might find yourself saying ‘I can’t do it’ or ‘I need an epidural’. If birth partners aren’t aware, they might start to panic at this stage too. It’s important they keep calm and reassure that you ARE doing it, you are amazing and powerful, and you will soon be meeting your baby.
The Second Stage – Pushing and Meeting Your Baby
The horizontal, inner muscles that were relaxing, and gathered upwards during the first or ‘up’ stage of labour, now have the job to push down, naturally easing the baby out through the fully dilated cervix. This is known as the second or ‘DOWN’ stage of labour. During this stage, if birth is safe and undisturbed, the “Ferguson reflex” may be experienced. This is a natural involuntary reaction where the pressure from the baby on your cervix and vagina creates an oxytocin boost which stimulates the uterus muscles to contract more powerfully. With the Ferguson reflex, you are likely to instinctively work with your body to push baby out.
In some, more rare cases, the birthing woman might experience the “Foetal Ejection Reflex”. This can happen due to a sudden surge in adrenaline which can result in an immediate ejection of the baby and therefore a very quick second stage. The foetal ejection reflex can happen as a response to fear but also in a state of physiological balance when birth is undisturbed, and the birthing woman has a complete release of inhibitions. If you experience the foetal ejection reflex, you will not feel like you are actively pushing, your baby will just be ejected from your body. Occasionally, this can happen when the dilation of the cervix is less than 10cm.
The second stage of labour can last up to 3 hours if you are giving birth for the first time and up to 2 hours if you have birthed before. However, this is just an average. Every woman is different, and your birth journey will be unique to you.

The Placenta Stage – What Happens After Baby Arrives
The third stage of labour is often forgotten about when birth is represented in films or on TV. Consequently, many women do not know there is a third stage – I certainly didn’t when I was pregnant for the first time!
So… what is the third stage of labour?
After your baby has been born, your body has to birth the placenta. You have created this amazing organ to nourish and grow your baby during pregnancy, but it a temporary organ and is now no longer needed. To release the placenta, your body needs to continue contracting, which means it must keep producing oxytocin. A calm, quiet, and private environment helps support this final stage of birth. The placenta can take 30-60 minutes to release in a physiological third stage. If you choose to have ‘active management’, where you receive an injection of synthetic oxytocin to help the uterus contract more quickly, it can take between 5-30 minutes.
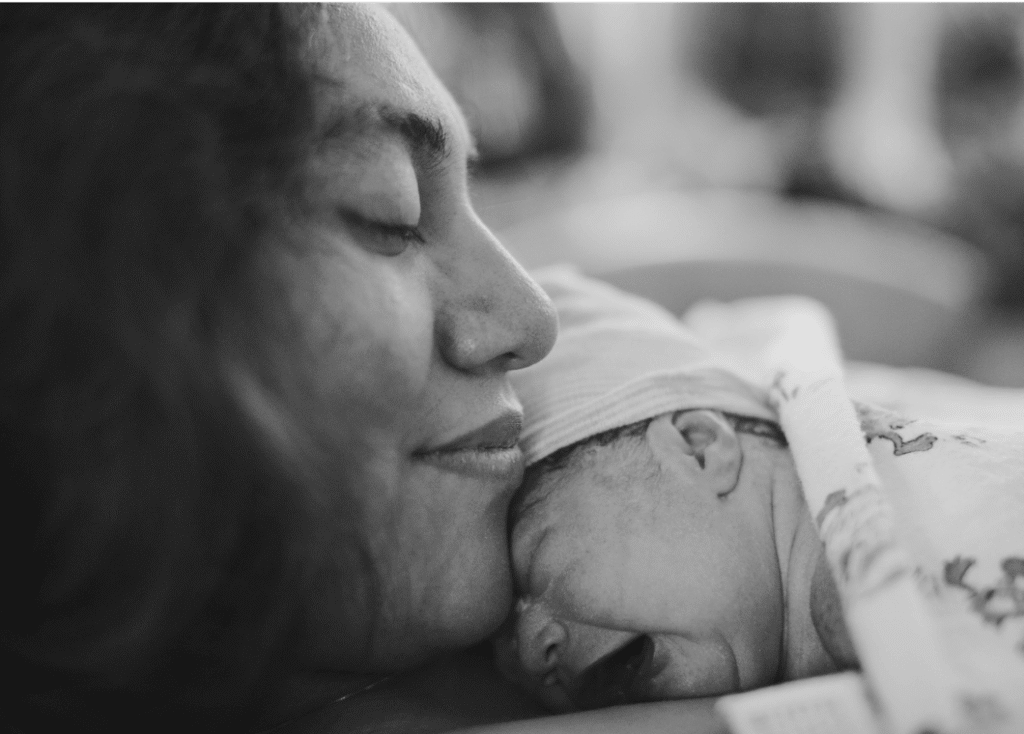
This ‘Golden Hour’ after birth is a time where your baby should have skin-to-contact with you. They will be adjusting to life outside of the womb and undergoing huge changes to adapt to life in the outside world. There are many benefits of skin-to-skin time immediately after birth for both you and baby. Don’t forget that you will also be experiencing hormonal changes during this time. There is no rush to weigh baby or call family and friends. You have grown, nurtured and birthed a baby – you are amazing! Give yourself some time to let that all sink in.
Writing birth preferences to help you explore your options for birth should form a key part of your pregnancy journey. Including a section about the third stage of labour is important to. It is during this part that you’ll be faced with further choices such as to whether to administer the Vitamin K injection to your baby.
Who Will Be Supporting You? Understanding Local Midwife-Led Care
What Community Midwives Cover in Devon & Cornwall
In Cornwall and Devon, community midwives are your key support throughout pregnancy, birth and the early weeks with your new baby. Your community midwife is likely to be the first person you speak to in detail about your pregnancy and someone who will be there to offer guidance and support throughout your pregnancy journey. Incredibly, Rosie, who was my lovely community midwife for both of my pregnancies, was also my mum’s midwife when she was pregnant with me!

Community midwives offer personalised antenatal care—checking your health and your baby’s growth, helping with screening choices and planning your birth—either at home, in local clinics or community hubs. After your baby is born, they will continue to support you with postnatal visits, feeding advice and checks for you and your baby before care transitions to health visitors and your GP. Wherever you’re planning to give birth, community midwives will support you and offer advice and reassurance.
What Happens at a Birth Centre vs Hospital Birth
If you choose to birth your baby in a birth centre, your care will be led by a team of midwives, who will provide continuous, hands-on support throughout your labour and birth. In a hospital setting, midwives remain your main caregivers but there will also be obstetricians, anaesthetists, and other specialists available if extra support is needed.
Wherever you give birth to your baby, it is likely to be your chosen birth partner who plays one of the most important roles. They will be the one who knows you best, who you trust and who can offer comfort, reassurance, and familiarity as you move through each stage of labour. Knowing they are there by your side is likely to have a significant impact on how you feel throughout your labour journey. Ensuring they know how they can support you best should be an important part of your preparation while you are pregnant.

When an Obstetrician May Be Involved
For many people, labour and birth progress smoothly under midwifery-led care and evidence shows that there is a lower chance of needing an intervention if you are supported by a midwife-led team*. Sometimes, though, an obstetrician may become involved to offer additional expertise or support. This might happen if labour isn’t progressing as expected, if there are concerns about you or your baby’s wellbeing, or if you need extra pain relief such as an epidural. Obstetricians are also involved if you choose to have an assisted birth or a caesarean section.
After the Birth: Postnatal Care in Cornwall & Devon
Local Midwife Visits and GP Check-Ups
After your baby is born, when you are ready, midwives will carry out checks on both you and baby and ensure you do not need any further care before you go home. If you have had a caesarean you will normally be advised to stay in hospital for 24 to 48 hours on the postnatal ward.
Your community midwife team will contact you the day after your baby’s birth or the day after you are discharged from hospital. If you have just given birth to your first baby, they will offer to see you on the first day after birth/after you come home. If you have had a baby before, they will discuss an individualised plan with you. You will then be offered appointments on day 5 and 10 where they will offer screening tests for your baby and weighing. Your care will move from the community midwife team to the local health visiting team, usually within the next 1-3 weeks following these appointments. At around 6-8 weeks after your baby’s birth, you’ll be invited to have a post-natal check with your GP. At this appointment, they will check in on your wellbeing and your physical recovery as well as checking your baby.
Don’t be afraid to ask questions and seek advice from your midwife, health visitor or your GP. They are there to support you. The early days and weeks of motherhood are incredibly daunting, particularly if you are a first-time mum. I remember feeling shell-shocked. I was shattered and felt like I had very little knowledge of how to look after a newborn baby, yet the responsibility I felt was overwhelming. Reaching out to your midwife/health visitor or a trusted family member or friend is not a sign of weakness. It is important to look after your own wellbeing as a new mum. Remember to ask for help if you need it.
Feeding Support in Your Area
For many, choosing whether or not to breastfeed isn’t an easy decision. Breastfeeding was so much harder than I thought it was going to be and I am so grateful for the support I had in the early days. Once we got into the swing of things and my nipples toughened up, I actually enjoyed the bond it created between me and each of my children. If I didn’t receive the support I did, I am not sure I would have continued past the first few days.
In Cornwall, we are very lucky to have an active network of local support to help you with breastfeeding, both before and after your baby arrives. Community breastfeeding peer support groups run in many towns and villages—like Bodmin, Bude, Launceston and Callington—offering drop-in sessions where you can chat with trained peer supporters and other parents while feeding your baby or getting ready to start feeding. These groups are supported by local health visiting teams and are a great place to build confidence and connect with others. To find out more about support in your area, click here.
There’s also an inclusive Breastfeeding Welcome scheme encouraging cafés, restaurants and other venues to show they’re happy to support mums feeding in public. This is something which not everyone is comfortable with when you are first starting out on your breastfeeding journey. It takes time to build confidence. Knowing there are places you go where you will feel safe and supported during feeding can really make a positive difference in the early days and weeks.
In Devon, you can access local and national resources to support your breastfeeding journey as well. There are feeding groups and networks such as Devon Positive About Breastfeeding, which help you find welcoming places to breastfeed and connect with other parents.
You’ll also find helpful information and helplines listed on NHS maternity sites, including the National Breastfeeding Helpline, La Leche League, Association of Breastfeeding Mothers and NCT Feeding Support, which offer practical advice by phone or online.
In addition to local services, you may choose to connect with specialist support if needed, including private lactation consultants and breastfeeding services in the region. Community hubs often host support sessions and are good places to connect with others. Whatever support you choose, seek support if you need it. Breastfeeding, although natural, doesn’t come naturally to many mums. Your wellbeing is important too. If breastfeeding isn’t working for you, talk to someone about how to transition to formula feeding. You must do what feels right for you and your baby.
Read my personal breastfeeding journey here.
Baby Groups, Antenatal Peer Meet-Ups and Parent Communities
There are many baby groups within Cornwall and Devon; looking at local community notice boards can be a good place for information on what is available in your area. Often, it can feel daunting to leave the house with a newborn, but connecting with other new mums can be such a positive experience. Many will make strong bonds and become life-long friends, others will appreciate the support and comfort in knowing they are not alone. If you are worried about attending a new group, my advice would be to take the plunge and give it a go!
If you live in the Launceston area, Francesca Parsons, a local newborn specialist, runs baby massage groups. Take a look at her Facebook page for more info: Natural Newborn

However and wherever you give birth to your baby, your birth journey will be unique to you. Taking time during your pregnancy to understand the birth process and how you can support it, as well as familiarising yourself with your options, is important. Your mindset as you go into labour can be vital in shaping your experience, as can your ability to make informed decisions around what happens to you and your baby. Remember, your body, your baby, your birth.
*http://evidencebasedbirth.com/evidence-inducing-labor-water-breaks-term/

I’m Demelza.
I am a mum to 2 energetic children, birth educator and former primary school teacher. I teach relaxation classes and hypnobirthing antenatal courses to pregnant mums and their birth partners in North Cornwall and West Devon. Birth preparation courses are also available online. Explore my website to find out more about the services I offer, or get in touch if you have any questions. I would love to support you in your preparation for a gentle and positive labour and birth.


